UMD graduate students studying to be speech-language pathologists (SLPs) had a powerful interprofessional learning opportunity last semester. A joint seminar had them working collaboratively alongside students from the College of St. Scholastica (CSS) who are preparing to be physical and occupational therapists.

The intent of the seminar, which happens each fall, is to better prepare all the students to serve their eventual patients. Lynette Carlson recognized several years ago that working in interdisciplinary teams could help her students become better practitioners. So the instructor in the UMD Department of Communication and Sciences Disorders (CSD) and director of the Robert F. Pierce Clinic reached out to faculty in physical and occupational therapy at CSS to create a collaborative educational experience.
The results have been overwhelmingly positive, according to CSD Associate Professor Sharyl Samargia-Grivette, who heads up the Neural Function and Recovery Lab and now coordinates UMD’s portion of the event. She says this interprofessional practice (IPP) opportunity helps drive home concepts students are learning in the classroom.
As part of their master’s program, CSD students learn about neurogenic communication disorders and the ways that stroke and brain injury can impact a person’s mobility and communication. After such traumas, SLPs help people with cognition and communication, including speech and the use and understanding of language.

The same patients also work with physical and occupational therapists. Physical therapy (PT) targets motor, balance and mobility while occupational therapy (OT) helps people safely accomplish aspects of daily living such as getting dressed, cooking and personal hygiene. Best practices have recently evolved to encourage professionals from these divergent but overlapping disciplines to coordinate care plans since such holistic treatment benefits patients.
Case Studies Encourage Collaborative Learning
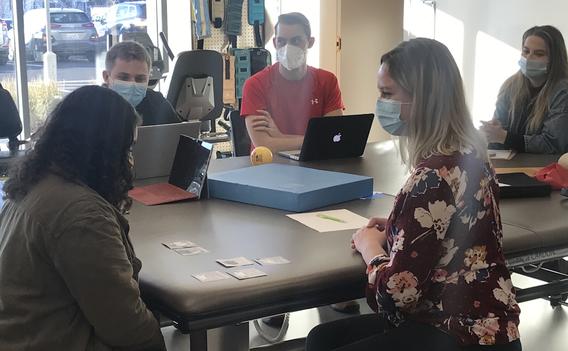
As part of the seminar, students are put into interdisciplinary teams and given elaborate mock case studies to work on. One features a client with a traumatic brain injury and the other includes one recovering from a stroke. The students all work together to evaluate and treat the clients.
A student reflection affirmed the value of such an exercise. “It was really interesting to see how all of the disciplines collaborated and how much overlap there was between disciplines. I noticed OT and speech did a lot of things with cognition which was really cool to see how they overlapped and how we approached activities. We would work on similar tasks but approach that task in a different way.”
Another student shared, “...I think this experience gave me a very positive outlook on interdisciplinary work and how it can benefit the patient in a multitude of ways. I also think it expands my own personal knowledge and allows me to incorporate maybe some more movement into my sessions being that movement is important for retaining information.”
Yet another participant commented on “how important it is for the three professionals, OT, PT, and SLP to communicate with each other. If there isn’t communication, it will affect the treatment of the client. As a professional, it is important to know the patient as a whole. Not only that, but it creates the idea of cotreatment and how beneficial it is because it can make more success in each area.”
Besides collaborative student learning, Samargia-Grivette says the seminar “is a great way for faculty and staff across programs and campuses to work together.” IPP education is also important because it has become a new accreditation standard required by many organizations. Most importantly, when professionals work well together, they can help patients achieve more.
“At the end of the day, our goal is the same—to get that person to be as independent as possible,” says Samargia-Grivette.
Additional faculty involved in the IPP seminar from the College of St. Scholastica: Associate Professor Alexandra Borstad, Assistant Professor Lynda Spangler (physical therapy), Assistant Professor Christine McConnell and Assistant Professor Jamie Hunter (occupational therapy).
